How I Met Your Mother fans power pediatric research
As Barney Stinson would say, “It’s gonna be Legen—wait for it—dary!” The beloved TV show How I Met Your Mother isn’t just about high-fives and blue french horns—it’s also making a real-world impact by fueling groundbreaking research in pediatric cardiology. The show supports the vital research led by Paul Grossfeld, MD, a pediatric cardiologist at Rady Children’s and a professor of pediatrics at UC San Diego School of Medicine.
In 2007, co-creator Craig Thomas’ son, Elliot, was diagnosed with Jacobsen Syndrome, a rare disorder caused by the deletion of a segment on chromosome 11. At the time, the outlook was bleak, and Craig and his wife, Rebecca, felt lost and helpless. In search of answers, they learned about Dr. Grossfeld’s work. He was one of the only researchers studying the condition, and his knowledge provided a lifeline and hope.
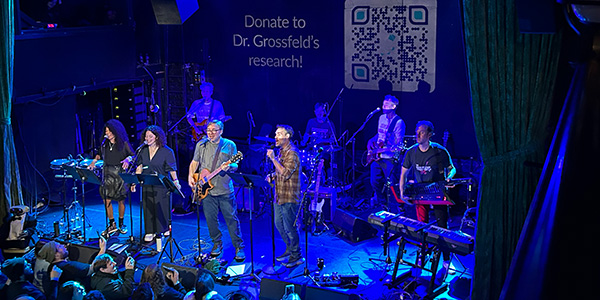
Fast forward 17 years, and Elliot is thriving and even playing the drums alongside his dad—all thanks to Dr. Grossfeld and the work of his team.
Driven by a desire to give back and with mom Rebecca leading the charge, the family organized fundraisers on the show’s set, rallying the cast and crew to raise awareness and money for research. Over the years, their efforts fueled breakthroughs in understanding and treating the syndrome.
“The support from How I Met Your Mother has been overwhelming,” says Dr. Grossfeld. “Craig and Rebecca, along with the entire cast and crew, have shown an outpouring of love and commitment to advancing our work. Even years after the show ended, Craig continues to host annual fundraising events.”
These funds have supported key initiatives, such as developing treatment protocols for preventing complications in children with Jacobsen Syndrome, including heart problems, bleeding disorders and infections. These protocols have been shared with medical professionals worldwide, significantly improving patient outcomes.
Unraveling the Genetic Mysteries of Severe Heart Defects
The connection between How I Met Your Mother and groundbreaking research highlights the importance of understanding why severe congenital heart defects happen. Dr. Grossfeld believes that to fully understand these heart problems, we need to find the genes that cause them and learn what those genes do.
Dr. Grossfeld’s interest in Jacobsen Syndrome began in the 1990s during his fellowship when he encountered a patient with hypoplastic left heart syndrome (HLHS), meaning the left side of his heart had failed to fully develop. The condition is fatal and currently has no cure.
Two decades earlier, researchers had discovered that Jacobsen syndrome was caused by a loss of genetic material on chromosome 11. Recognizing a potential link between Jacobsen syndrome and HLHS, Dr. Grossfeld saw an opportunity to explore the genetic underpinnings of congenital heart disease.
“Back then, we had limited tools,” Dr. Grossfeld recalls. “It was an observation, and I had no idea how to pursue it further. But with advancements in genome sequencing technology, we can now pinpoint specific genes and investigate their roles in heart development.”
By combining genetic insights with functional studies, Dr. Grossfeld’s research seeks to bridge the gap between genetic causes and their physiological manifestations, ultimately aiming to improve clinical care for affected children.
Looking to the Future: Advancing Research and Precision Medicine
“Using advanced genetic tools and animal models, we are beginning to understand how these genes interact and cause the condition.”
—Dr. Paul Grossfield
Dr. Grossfeld’s research has come a long way, but he acknowledges that there is still much work to be done.
“We have identified two genes involved in the development of HLHS, but we now believe an additional gene on chromosome 11 plays a critical role,” Dr. Grossfeld explains. “Using advanced genetic tools and animal models, we are beginning to understand how these genes interact and cause the condition.”
Looking ahead, the research team is embarking on an exciting new phase: studying patient-derived cells to develop personalized treatment strategies. By using cardiac organoids— miniature heart models grown in a petri dish—as well as bioengineered cardiac tissue, they aim to predict how individual patients will respond to therapies, paving the way for precision medicine.
Dr. Grossfeld collaborates with institutions like UC San Diego, Sanford Burnham Prebys and Georgia Tech to push the boundaries of what is known about HLHS and related diseases.
Reflecting on his journey, Dr. Grossfeld finds the intersection of science and personal relationships to be the most rewarding aspect of his work.
“Our team has more insight into this disease than any other group in the world, and that is exhilarating. But the relationships I’ve built with families globally are what truly enrich my life,” he says. “Hearing that the information we’ve provided has given them hope or even saved their child’s life is incredibly fulfilling.”
To learn more about Dr. Grossfeld’s research and how you can help, visit https://fundraise.radyfoundation.org/miracle-makers/dr.-paul-grossfeld-heart-research-fund.
To learn more about Rady Children’s Division of Cardiology, visit https://www.rchsd.org/programs-services/cardiology/.